This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 55 yr old female came to the casualty with chief complaints of
Fever since 20 days which is on and off ass with chills subsided on medication
Vomiting
Burning micturation
Pain abdomen colicky pain on and off since 20 days
Loose stools ( 2 -3 episodes/ day)
HOPI
Patient was apparently asymptomatic 4 months back then developed pain abdomen , non radiating , colicky type associated with nausea vomiting and was taken to local doctor for which investigation were done and was diagnosed as abscess and was treated approximately since 20 days she developed pain abdomen colicky pain on and off since 20 days , burning micturation from 1 day she has loose stools ( 2 -3 episodes/ day)
Known case of DM type 2 since 11 days and is on Tab Glimi M1 OD
Not a know case of HTN /Asthma /TB/Epilepsy
On examination
General
Pallor -ve
Cyanosis -ve
Icterus - ve
Clubbing - ve
Lymphedenopathy -ve
Oedema - ve
Mild dehydration present
Temp 98.7 ⁰ F
PR 84 BPM
RR 18 cpm
Spo² 84 % at room temperature
95 % on 5 lit of oxygen
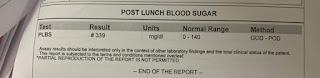
Grbs 395 mg%
Systemic examination
CVS
S1 S2 heard.
No thrills or murmurs
RS
BLAE+, NVBS
P/A : Soft, tender , no palpable mass
CNS
NAD
Provisional diagnosis
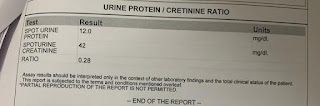
Pre Renal AKI 2⁰ to recurrent UTI
associate Denovo DM type 2
Chest xray
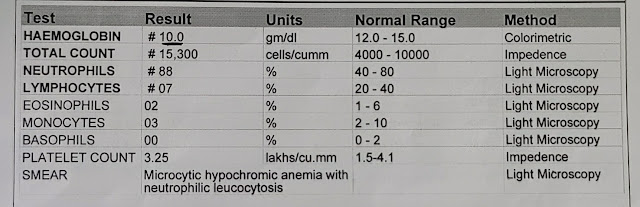
CBP
Abg
USG
Day 1 treatment plan
W/H OHA till further orders
2) GRBS 6th bouly pre-meal
3) INJ HAI S/c pre-meal / FID
4) Foley's catheter
5) IUF- NS @ U·0+ 30ml/hr
6) INJ PANTOP 40mg IV OD.
3) INJ ZOFER 4mg 110/BD
8) ORS sachets 200ml after each episode.
9) Inj CEFTRIAXONE 1gm IV BD
Day 2
Hemogram
RFT
2d echo
Day 2 update
1 NS @ UO + 30ml/hr
2 Inj ceftriaxone 1 gm iv bd
3 inj pantop 40 mg od
4 ors after each episode
5 inj HAI
6 grbs charting 6 hrly