1601006064
This is my short case where a
50 year old female came to the OPD with
CHIEF COMPLAINTS-
Pain
Stiffness in several joints since one year
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic 10 years ago thent she developed a dull aching type of pain and stiffness in her metacarpophalangeal joints in her right hand associated with limitation of movements at the joint .
Then within 6 months of the onset of the disease, it has progressed to involve other joints of the right hand,left hand as well as wrist and elbow joint
Then within 4 years of onset she started feeling pain in the joints of feet and ankle
Since 3 months the pain became unbearable limiting her activities.
PAIN was insidious in onset,slowly progressive,dull aching type of pain,non radiating,associated with swelling ,stiffness and limitation of movements in the involved joint.
STIFFNESS and PAIN was more in the first one hour of waking up and gradually improved with movements
No deformities
No loss of weight
PAST HISTORY-
She has no similar complaints 10 years ago
No history of thyroid ,asthma,diabetes,TB,epilepsy , HTN
MEDICAL HISTORY-
She has no similar complaints 8 years ago.
No history of thyroid, Asthma, hypertension, diabetes
DRUG HISTORY-
No known drug allergies
MENSTRUAL HISTORY-
Menarche - 13 years
She has regular cycles of 29 days duration
Menopause - 47 years
FAMILY HISTORY-
No significant family history
PERSONAL HISTORY-
Diet - mixed
Appetite - normal
Bowel and bladder movements - regular
Sleep - adequate
No Addictions
GENERAL EXAMINATION-
Patient is conscious,coherent,cooperative
Moderately built and nourished
No pallor
No icterus
No cyanosis
No clubbing
No lymphadenopathy
No Edema
VITALS-
Temperature - afebrile
Blood pressure - 115/70 mm Hg
Respiratory rate - 15 cycles / min
Pulse - 70 bpm
LOCAL EXAMINATION
INSPECTION
Skin-No subcutaneous nodules
No pigmentation
No scars
No atrophic changes
No purpura
No ulcerations
No gangrene
Nail-Normal
Soft tissues -Swelling over the joints
Deformities- No deformities in hands and feet
PALPATION-
Skin - warm
Sensations are present
Soft tissues- no edema
Joint capsule - mild swelling over the joint
Tenderness over the joint
Movements - decreased range of movements at PIP,MCP,wrist,elbow,ankle joints
All active and passive movements at the involved joints are painful
No crepitus
SYSTEMIC EXAMINATION-
CVS
Apex beat - 5th intercostal space lateral to midclavicular line
S1 S2 heard
JVP normal
Pedal edema - absent
RESPIRATORY SYSTEM-
Breath sounds - normal
No additional breath sounds
CNS-
Sensations - preserved
Joint position sense - intact
Gait - normal
Cranial nerves -intact
Reflexes - preserved
ABDOMEN -
No abnormal findings found
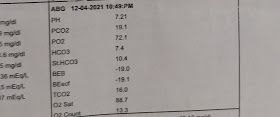
INVESTIGATIONS-
-Complete blood picture
-ESR
-CRP
-Rheumatoid factor
-Anti nuclear antibodies
-Liver function test
-Urine examination
PROVISIONAL DIAGNOSIS:
RHEUMATOID ARTHRITIS
TREATMENT
1.Prednisolone
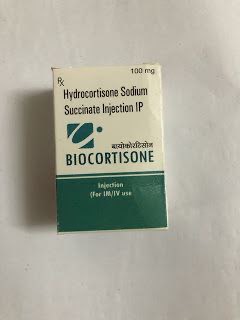
2.Hydrocortisone sodium
3. Tramadol